Meet Our Keratoconus Specialist in Ft. Lauderdale, Florida
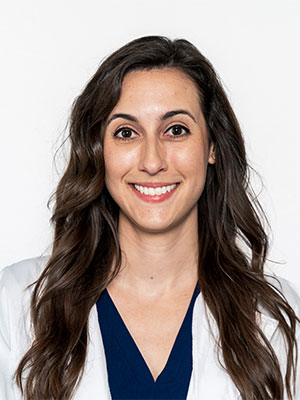
Dr. Panagos earned a Bachelor of Science degree in Psychology at Florida State University. She then attended Nova Southeastern University College of Optometry where she earned a second Bachelor of Science degree in Vision Science and her Doctor of Optometry degree. Dr. Panagos is the recipient of the 2020 Eschenbach Award of Excellence in Low Vision and was inducted into the Beta Sigma Kappa Honor Society.
She was selected for a post-doctoral residency at the Orlando VA Medical Center in Hospital Based Primary Care Optometry and Ocular Disease. She received specialized training in traumatic brain injuries, low vision rehabilitation, and specialty contact lenses. Dr. Panagos is proficient in the medical managment of glaucoma, diabetic retinopathy, and macular degeneration. She has a passion for scleral contact lenses and ortho-keratology.
Dr. Panagos is a Fellow of the American Academy of Optometry. She is member of the National Keratoconus Foundation and International Keratoconus Academy. She is a member of the American Optometric Association, Florida Optometric Association, and serves on the board of the Palm Beach County Optometric Association. She enjoys cooking, playing tennis, and cheering on the Seminoles!

Dr. Bascome was born and raised in Fort Lauderdale, Florida. He earned his bachelors degree in Biology from Nova Southeastern in 2006 and went on to graduate with clinical honors in ocular disease and primary care from Nova Southeastern College of Optometry in 2010. While in optometry school, Dr. Bascome received an award for demonstrating superior clinical skills and excellence in the diagnosis and treatment of ocular disease. His clinical interests include, Specialty Contact Lenses, Dry Eye and Glaucoma Management. Dr. Bascome joined Broward Eye Care in 2012 and enjoys helping the community he grew up and still lives in. He believes in providing personalized care using state of the art diagnostic technology. When he is not spending time with patients, Dr. Bascome enjoys spending time with his family and playing golf. He is enthusiastic about his career and is anxious to fulfill your optometric needs.
Academic
- Adjunct Professor Salus University College of Optometry
- Adjunct Professor Massachusetts College of Pharmacy & Applied Sciences
- Fellow American Academy of Optometry- Candidate
- Fellow of the Scleral Lens Education Society-Candidate
Profession/Member Associations
- American Academy of Orthokeratology and Myopia Control
- Scleral Lens Education Society
- International Keratoconus Academy
- American Optometric Association
- Florida Optometric Association
- Broward County Optometric Association.
- Cardinal Gibbons Alumni Association
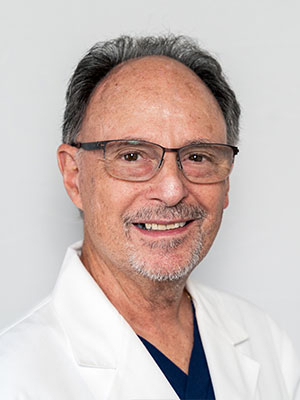
Paul Klein OD is a 1979 graduate of the New England College of Optometry. Dr. Klein is in private group practice specializing in contact lens care, laser vision correction, and therapeutic optometry in Fort Lauderdale, Florida. He is a Fellow of the American Academy of Optometry, and a Diplomate of the American Board of Clinical Optometry.
Dr. Klein is the founding editor of Optometry Today magazine and is an Adjunct Professor of Optometry at the SALUS University, Pennsylvania College of Optometry.
Dr. Klein’s professional achievements include President of the Broward County Optometric Association, Chair of the American Optometric Association Contact Lens and Cornea Section, and election to the National Academies of Practice.
Dr. Klein has lectured and published nationally and internationally at various conferences and symposia. In addition he has participated as an investigator and consultant for numerous investigative clinical trials of contact lenses and contact lens care solutions.
Our Doctor Can Diagnosis and Treat Keratoconus
Your cornea is the transparent, outer lens of your eye, and it typically has a smooth dome shape. Keratoconus describes a condition in which the corneal structure isn’t strong enough to maintain a healthy ball shape.
Meet with our Keratoconus Specialist in Ft. Lauderdale, Florida to define your eye's condition and ways for treatment.
As a result, the cornea bulges outward into more of a cone. Our professional optometric team at our eye care clinic is knowledgeable about how to diagnose and treat keratoconus.
Keratoconus is rare, with an estimated one person out of every 2,000 having the condition. It generally appears in the teenage years and can progress slowly or rapidly.
Keratoconus also runs in families, so if you or your children are at risk, it’s advised to contact us for a thorough eye exam.
Causes of Keratoconus
Your cornea is held in place by very small collagen fibers. When they are weakened and too fragile, they aren’t able to preserve the round shape of your cornea.
A reduction in the protective antioxidants of your cornea, which act to destroy damaging by-products made naturally by corneal cells, is what causes keratoconus.
In addition to genetics, some types of eye injuries may increase your chance of being diagnosed with keratoconus.
Specific ocular diseases, such as retinitis pigmentosa, vernal keratoconjunctivitis and retinopathy of prematurity, as well as some systemic conditions (Down syndrome, Ehlers-Danlos syndrome, Leber's congenital amaurosis and osteogenesis imperfecta) are also associated with this corneal abnormality.
Our Keratoconus Specialist in Ft. Lauderdale, Florida has years of experience identifying the various levels of keratoconus and other corneal conditions.

Symptoms of Keratoconus
When the shape of your cornea begins to bulge, it alters your eyesight in two different ways. As the cone shape forms, your normally smooth corneal surface becomes wavy, called irregular astigmatism. Additionally, as your cornea expands, vision becomes increasingly nearsighted. Focusing becomes impossible without eyeglasses or contact lenses. Usually, the problems begin in one eye and develop later in the other eye too.
Typically, patient’s eyeglass prescription will change often as the vision becomes worse and contact lenses will be difficult to wear due to discomfort and improper fit.
When keratoconus become more severe (which usually takes a long time however on occasion can happen rather quickly), the cornea can begin to swell and form scar tissue. This scar tissue can result in even further visual distortion and blurred vision.
Altogether, these changes can create the following symptoms:
- Blurred vision
- Streaking of lights
- Halos around bright lights at night; glare
- Sudden change of vision in only one eye
- Objects appear distorted, both near and distant
- Double vision from just one eye
- Triple ghost images
How We Diagnose Keratoconus
Our eye doctors will inspect carefully for the signs of keratoconus during your comprehensive eye exam. It’s critical to inform us of any symptoms that you’ve been experiencing. To diagnose the condition, we’ll measure the shape of your cornea. Computerized Corneal Topography is used for this procedure, which takes a picture of your cornea and analyzes it instantly.
